Wake Windows vs. Sleep Schedules: Which One Should You Follow?
On the internet, you’ll see a lot of variable information. That’s just the nature of bias but also a wide range of definitions. A lot of people aren’t forthcoming with exact definitions to specific things like sleep training which can lead to confusion for a lot of parents. So before we dive in, let me explain how I use the terms in my work with clients:
Wake windows = the amount of time your baby is awake between naps (or between waking up in the morning and bedtime).
Sleep schedule (or “by the clock” schedule) = fixed nap times and bedtime each day, regardless of how “awake enough” the baby seems.
There is no one-size-fits-all answer. The right approach depends on your baby’s age, temperament, and your family’s goals. I’ll walk you through realistic ranges, what research (or lack thereof) says, and how to combine both in a way that makes sense for your baby.
What science (and experience) tell us
Wake windows: what they are and typical ranges
Wake windows are simple in concept, but their precision is more art than science. They’re based on acute sleep pressure: the longer your child is awake, the more tired they become, until they’re ready to nap.
This is a helpful, age-based guide:
Newborns (birth to 1 month): ~0.5 to 1 hour awake
1–3 months: 1 to 2 hours
3–4 months: 1.25 to 2.5 hours
5–7 months: 2 to 4 hours
7–10 months: 2.5 to 4.5 hours
10–12 months: 3 to 4 hours
Newborns might do 30–90 minutes awake; by 4 months, 1.5–2.5 hours are common; by 12 months, 3–4 hours is typical.
One caveat: researchers point out that there’s no definitive empirical data proving that babies must adhere to strict wake windows. ParentData notes that because of the challenges in defining and measuring “right awake times,” it’s unlikely we’ll ever have a perfect study on this. (ParentData by Emily Oster)
Wake windows do give you a ballpark to avoid two extremes: putting down too early (under-tired) or stretching too far (overtired). Overtiredness can lead to fragmented sleep, more night wakings, and harder settling.
(And wake windows are calculated by figuring out the average sleep needs for that specific age, subtracting from 24 hours to get their recommended total awake time, then dividing that between the number of naps/awake periods they need. Since every child’s sleep needs will vary, this is what makes wake times more volatile.)
Sleep schedules (by the clock): pros and when they become helpful
A schedule approach says: today we’ll nap at 9 a.m., 1:30 p.m., and bed at 7 p.m., give or take. You prioritize consistency over acute cues.
Supporters of schedules argue:
They help reinforce your child’s circadian rhythm (their internal clock) over time.
Predictability makes your life easier (planning errands or coordinating with caregivers becomes simpler.)
Over time, babies benefit from having stable nap and bedtime windows.
Some sources suggest that after 6 months or when your child settles into two naps, a clock-based schedule tends to become more effective. Other sources may recommend a hybrid: a schedule with small “variance windows” (e.g. 15 minutes) instead of rigid times.
The research is thin on one method outperforming the other. But one Pediatrics paper (on breastfed babies) showed that simple scheduling tweaks (like a dream feed between 10 p.m.–midnight) and consistent responding to nighttime waking, mproved infants’ stretch to 5 hours of consolidated sleep in 3 weeks (versus 23% in a control group). That supports the idea that some gentle scheduling has value.
Also, more recently, a mathematical sleep model (Homeostat-Circadian-Light Model) shows how external light schedules and consistency (versus weekend shifts) influence nighttime sleep consolidation. Irregular schedules significantly worsened nighttime waking in the model. (arXiv)
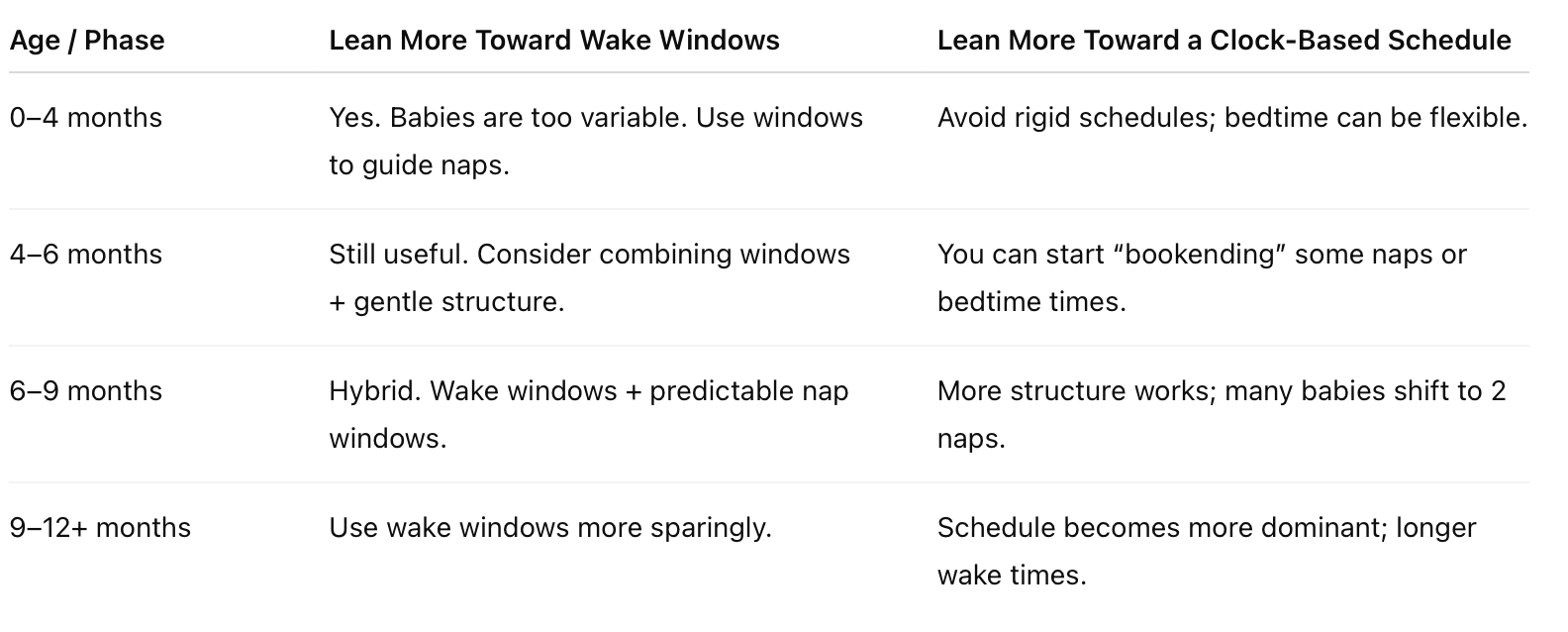
Wake Windows vs. Schedule: When to lean one way or the other
Here’s a rough guide (based on experience + literature) to when each method may be more helpful:
Some might find the best approach to be a hybrid; you use wake windows to gauge what’s reasonable, but you anchor some nap times and bedtime with consistency (within a 15–30 minute flexibility).
How I apply this approach with clients
Here’s how I guide families:
Start with wake windows for younger babies. Especially under 5 months, babies are more driven by acute sleep pressure than clock time. Use wake windows as your backbone.
Log and experiment for 1–2 weeks. Track naps, wake windows, bedtimes. See patterns emerge. Babies often self-settle into a rhythm.
Anchor one “fixed point” per day. Maybe first nap or bedtime has a fairly consistent time. That gives a sense of predictability.
Be flexible but consistent. If baby is clearly tired earlier one day, put them down early. If they seem alert, stretch slightly (within safe bounds).
Gradually shift toward schedule as they mature. As your baby hits nap transitions or moves to 2 nappable wake periods, you shift more structure.
Watch signs of overtiredness or “spilling”. If naps start compressing, nights start fragmenting, that’s your cue to adjust back.
One key belief I emphasize with clients: babies can learn independent sleep early if given the chance and uninterrupted naps and consolidated nights come from good day habits. That’s what I teach, not “cry it out.” You’re always responding, supporting, and gently guiding.
Tips to make either approach work better (realistic tweaks)
Use a 10–15 minute “variance window.” For nap times, allow ±10–15 minutes around your ideal time. This prevents sleep battles when small shifts happen.
Track for trends, not day to day. If baby slept poorly one day (illness, travel, developmental leap), don’t overreact. Look at 3–5 day trends.
Watch your light exposure. Morning light helps set circadian rhythm. The sleep model suggests irregular “light schedules” (e.g. weekend shifts) worsen nighttime wakings. (arXiv)
Respond to baby signals. Yawning, rubbing eyes, losing interest in play = signs it’s time to begin drifting toward nap. Don’t fight obvious cues.
Use consistent routines. A nap “prep routine” and a bedtime routine help cue sleep, regardless of whether you’re on windows or schedule.
Ease transitions gradually. When shifting from 3 to 2 naps, stretch windows slowly by 10–15 minutes over days, watching the baby’s response.
Adjust when needed. Growth spurts, illness, travel, they all throw things off. Temporarily lean back on flexibility.
What clients say about Heaven Sent Sleep
I believe results speak louder than promises. Here are real reviews from parents who’ve trusted our process:
“Heaven Sent Sleep was extremely quick to respond to my questions and always answered them thoroughly. She helped us to get him sleeping independently at night and naps … by the end I felt confident in how to support my son to get the sleep he needed.” (Heaven Sent Sleep)
“They provided amazing non-judgmental support … gave me great information on how to deal with upcoming challenges … I’m a better mom now.” (Heaven Sent Sleep)
“On our call, Lauren’s tips produced dramatic difference the very first night. It was life changing.” (Heaven Sent Sleep)
Final thoughts (from me to you)
There’s no perfect formula. If someone tells you rigidly that “wake windows are all you need” or “only schedules work,” they’re overselling certainty. Sleep is beautifully messy and adaptive.
What I do believe is this:
Use wake windows as your guide when baby is young.
Anchor one or two consistent times so you don’t live in total chaos.
Gradually shift to more structure as the baby matures.
Watch for signs of overtiredness or pressure.
Be kind to yourself, adjust when needed.
If you’re ever feeling stuck, second guessing, or just too exhausted to parse these decisions, I’d love to help you create a plan you feel good about. You don’t need to go it alone.